If you want to optimize your heart health and cholesterol, diet is the first place to start. It may seem simple enough: cut the carbs and fats, increase plant protein, and look for products labeled “heart healthy”. Yet, some of these seemingly healthy tips may do the opposite for your heart! The evidence on others is mixed, and a handful are indeed beneficial. Read on as we untangle the data to help you understand what you should actually be eating.
Disclaimer: This post is for informational purposes only. Please consult your doctor about your health-related concerns and medications before taking any supplements or making drastic changes to your diet and lifestyle.
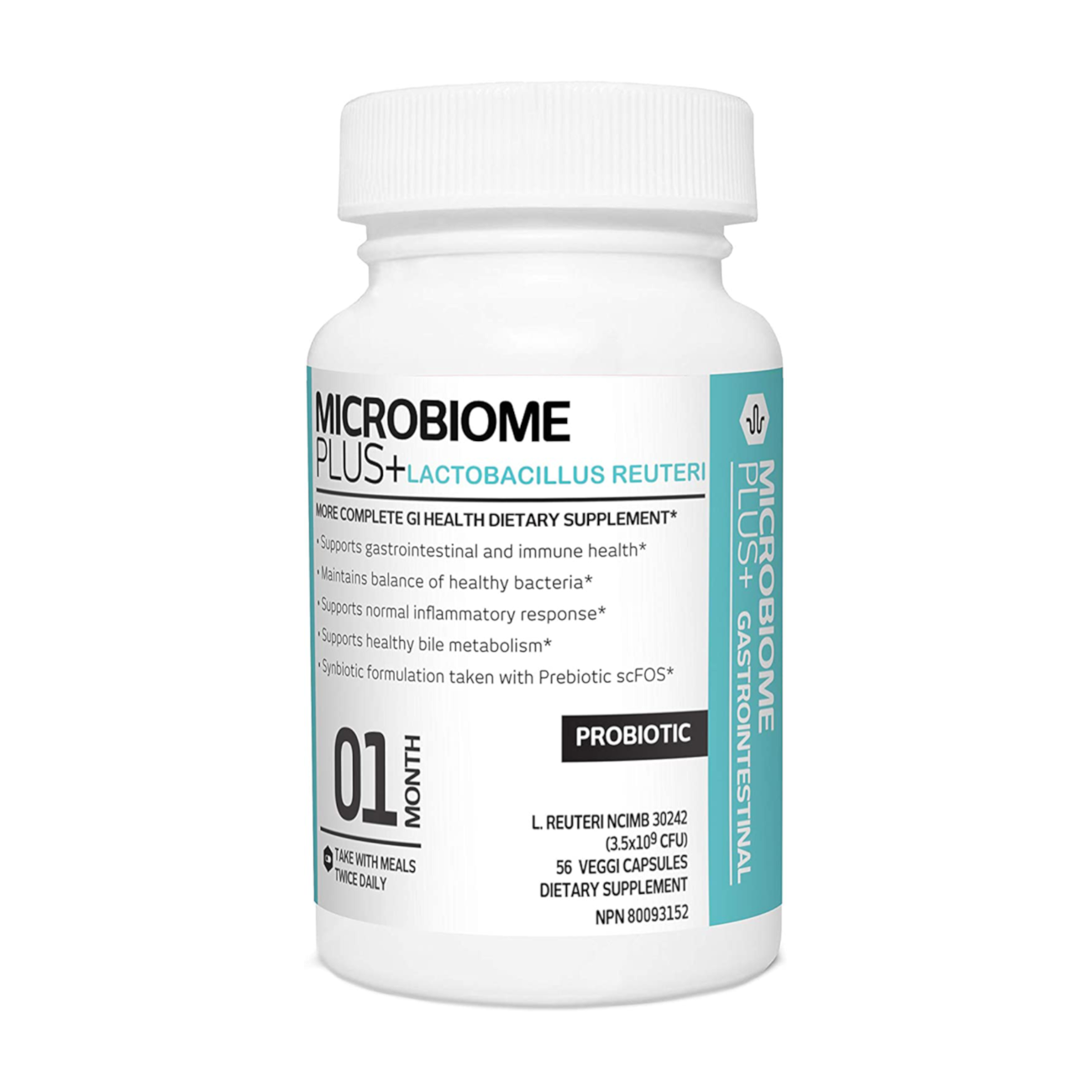
Buy Heart-healthy L. reuteri Probiotics
What is the Heart Healthy Diet?
Official AHA guidelines & metrics
Each year, the American Heart Association AHA issues an updated document with the latest statistics on cardiovascular disease, its risk factors, and strategies to achieve cardiovascular health. Among the key strategies is diet (Tsao et al., 2022).
According to AHA, a healthy dietary pattern is made up of five primary metrics (categorized as either beneficial or harmful):
- Fruits and vegetables (beneficial)
- Fish and shellfish (beneficial)
- Whole grains (beneficial)
- Sodium (harmful)
- Less sweet sugar beverages (harmful)
AHA also defines three secondary metrics:
- Nuts, seeds, and legumes (beneficial)
- Processed meat (harmful)
- Saturated fat (harmful)
Based on these eight metrics, each person’s dietary score is calculated. When a person hits most of these targets (≥80%), their score will be considered ideal. It’ll be intermediate if they somewhat meet the targets (40% to 79%) and poor if they mostly don’t (<40%).
Now, this score may seem simple enough. It was used in large scientific analyses, but only one study evaluated its effectiveness (Cacau et al., 2022).
Typical American diet statistics
- According to NHANES (National Health and Nutrition Examination Survey; 2015–2016), <10% of adults met the guidelines for whole grains (≥3 servings per day), whole fruits (≥2 cups per day), and nonstarchy vegetables (≥2.5 cups per day) (Belardo et al., 2022).
- According to the AHA primary diet score, 47.8% of US adults had poor diet quality in 2015 to 2016 (Tsao et al., 2022).
- On the basis of the AHA secondary score, 36.4% of US adults had poor diet quality in 2015 to 2016 (Tsao et al., 2022).
- More than any individual food or dietary restriction, food quality—macro and micronutrient density—seems to be the most important factor in determining how heart-healthy a diet is (Vanegas et al., 2022).
So, what is the ideal, heart-healthy diet? And why aren’t national and international guidelines keeping track of the latest research when making recommendations?
AHA dietary score limitations
Going only by AHA’s heart-healthy diet metrics has several limitations.
Many foods are lumped into the same categories without taking into account their quality and complex nutrient and heavy metal profiles. For example, canned tuna and wild-caught salmon don’t have the same nutrient profile or health effects. Neither does an ultra-processed vegan sausage and a fresh, organic, chickpea salad (Ohlau et al., 2022).
To add, some metrics are not based on good scientific evidence. The two most glaring examples are AHA’s recommendation to limit saturated fats and the FDA’s approval of plant sterols for reducing heart disease risk (Astrup et al., 2021; Helgadottir et al., 2020).
More holistic diet scores take into account the quality of macronutrients, the diversity of micronutrients, and the intake of ultra-processed foods (Cacau et al., 2022; Vanegas et al., 2022).
The Heart Healthy Diet & List of Foods
1) Increase fruits and vegetables
Scientific data confirms that high fruit and vegetable intake is beneficial for heart health.
The intake of 5 servings of fruit and vegetables per day (versus 2 servings) was recently linked with 13% lower total mortality, 12% lower heart disease mortality, 10% lower cancer mortality, and 35% lower respiratory disease mortality (Tsao et al., 2022).
Studies identified low fruit/vegetable intake as a major modifiable factor associated with heart attacks (Belardo et al., 2022).
Eat the rainbow
Were you ever told to “eat the rainbow” as a kid? There’s valid science to back it up!
The antioxidants and other phytonutrients that are packed into fruits and veggies tend to be vividly colored. Phytonutrients have widespread beneficial health effects. Upping your intake of colorful fruits and veggies ensures good heart health and nutrient diversity. Different-colored plants tend to have phytonutrients that benefit different organ systems (Minich, 2019).
The most beneficial phytonutrients for the heart are typically colored green, for lowering inflammation red, and for the brain and blood circulation blue-purple (Minich, 2019).
Food list
Here are some fruits and vegetables to aim for every day (Minich, 2019):
- Green foods: avocado, Brussels sprouts, green tea, olives, artichokes, asparagus, broccoli, celery, leafy greens, lentils, green peas, snap peas
- Red foods: apples, blood oranges, pomegranate, raspberries, red currants, red beets, red bell peppers, red onions
- Purple foods: blackberries, blueberries, purple grapes, eggplant, purple kale, purple potatoes, purple cabbage, black beans
According to a meta-analysis, eating cruciferous and green leafy vegetables almost every day could reduce heart disease risk by ~16% (Pollock, 2016).
Garlic is a curious case. It’s white but contains phytonutrients from all color categories. Many studies back up its benefits for heart health and cholesterol (Minich, 2019; Ried et al., 2013; Varshney & Budoff, 2016).
2) Get plenty of fiber and whole grains
Greater dietary fiber intake is associated with a lower risk of cardiovascular disease and coronary heart disease. The evidence is aligned with general recommendations to increase fiber intake (Threapleton et al., 2013).
Many fruits, vegetables, and legumes covered in the previous section are also high in fiber.
Plus, fiber acts as a prebiotic, fueling your good gut bacteria. It also helps maintain healthy cholesterol levels and boosts your gut microbiome (Soliman, 2019; Oniszczuk et al., 2021).
Similarly, eating more whole grains reduces the risk of heart disease and other chronic diseases, according to a meta-analysis of 45 studies. Whole grain intake was associated with a reduced risk of coronary heart disease, cardiovascular disease, cancer, and dying from any cause (Aune et al., 2016).
Food list
Consider adding the following whole grains to your diet:
- Oatmeal
- Barley
- Brown/wild/black rice
- Buckwheat.
- Bulgur
- Millet
- Amaranth
- Spelt
3) Eat food rich in probiotics
Prebiotics and probiotics help keep your gut microbiome healthy. Gut microbiome dysbiosis happens when this balance is disrupted.
Gut dysbiosis can cause many acute or chronic cardiovascular problems. Research unveils that intestinal microbiota imbalances and inflammation play a big role in the development of heart disease (Wu & Chiou, 2021).
Food list
Probiotics are found in many healthy fermented foods, such as:
- Yogurt, kefir, and fermented milk
- Cheese (such as blue cheese, camembert, and asiago)
- Kimchi and sauerkraut
- Olives
- Fermented fish
- Miso
- Kombucha
Although increasing the intake of dietary probiotics is beneficial, probiotic effects are strain-specific.
L. reuteri NCIMB 30242 is the best-researched probiotic specifically for heart health and cholesterol. It supports healthy total and LDL cholesterol levels and has been through 7 clinical studies (Jones et al., 2011, Jones et al., 2012; Jones et al., 2013, Jones et al., 2013; Martoni et al., 2015; Jones et al., 2011; Jones et al, 2012).
Buy L. reuteri Probiotics with Prebiotic Fiber
4) Find healthy sources of fat
The mainstream recommendations get controversial with dietary fats and dairy.
You probably think you should be eating a low-fat diet and carefully limiting your saturated fat intake to keep your heart healthy, right? And that is what most experts will tell you. Except—the data doesn’t add up.
Your food matrix matters.
First off, dietary fat quality is more important than total dietary fat intake (Guasch-Ferré et al., 2015).
Just counting saturated fat fails to see the bigger picture: what’s the overall dietary pattern of this person? Are they getting enough nutrients? What’s their food matrix like? (Astrup et al., 2021).
In a large randomized trial among patients with heart disease risk factors, unrestricted-calorie Mediterranean-style diets supplemented with extra-virgin olive oil or mixed nuts reduced the risk of stroke, heart attack, and death from cardiovascular causes by ~30%, compared to a reduced-fat diet (Estruch et al., 2018)
According to a recent AHA publication, people with higher intakes of total fat, polyunsaturated fatty acids (PUFAs), and monounsaturated fatty acids (MUFAs) had lower total mortality. The data on saturated fats was mixed (Tsao et al., 2022).
Whole-fat dairy, unprocessed meat, and dark chocolate are foods rich in saturated fats with a complex matrix that are not associated with an increased risk of heart disease (Astrup et al., 2020).
Research on full-fat dairy products high in saturated fat, particularly fermented dairy foods, revealed some benefits for cardiometabolic diseases (Dehghan et al., 2018).
Saturated fats are not downright bad.
Nearly 20 papers recently reviewed the data on saturated fats and cardiovascular outcomes. They concluded that there’s a lack of rigorous evidence to support continued recommendations either to limit saturated fats or to replace them with polyunsaturated fatty acids. Yet, these papers were not considered when making the most recent U.S. Dietary Guidelines for Americans (Astrup et al., 2021).
One study linked the replacement of animal fats, including dairy fat, with vegetable sources of fats and PUFAs with a reduced risk of cardiovascular disease. Other analyses found no link or no beneficial effects of reducing saturated fat intake on heart disease and total mortality, and instead found protective effects against stroke. Several analyses had inconsistent findings (Chen et al., 2016; Astrup et al., 2020; Heileson, 2020).
Saturated fats seem to increase low-density lipoprotein (LDL) cholesterol due to increasing levels of larger LDL particles that are less strongly related to heart disease risk (Astrup et al., 2020).
PUFA-rich vegetable oils, on the other hand, may lower total cholesterol and LDL but at the expense of more reactive LDL. The PUFAs that get incorporated into LDL are more susceptible to lipid peroxidation, which causes atherosclerotic buildup in blood vessels (Lawrence, 2021).
Despite lacking and conflicting evidence, the current guidelines still recommend limiting saturated fats to 10% or less of total energy intake (Astrup et al., 2021).
Data on dietary cholesterol is mixed.
Our cells need cholesterol to function. US 2020 guidelines now state that healthy dietary patterns are “lower in cholesterol”, but a systematic review by the USDA itself says that there is “insufficient evidence” to link the intake of dietary cholesterol with cholesterol levels in the blood (Astrup et al., 2021).
Also, the all-cause death rate is higher in humans with low compared with normal or moderately elevated serum total cholesterol (Lawrence, 2021).
Genetics play in.
There are large individual differences in how each person responds to saturated fat, cholesterol, and PUFAs from food. Many of these differences have a genetic basis (Krauss & Etherton, 2020).
Polyunsaturated fats or PUFAs are a great example. PUFAs are found in diverse foods, from nuts and seeds to fish to vegetable oils (including highly processed industrial oils like canola, rapeseed, corn, sunflower, and soybean oil).
Your body uses PUFAs for nerve function, blood clotting, brain health, and more. Beneficial in the right amounts, PUFAs become toxic in excess. They can be oxidized and turned into highly reactive, inflammatory compounds (Lawrence, 2021).
Genetic variations that affect blood cholesterol levels often also affect PUFA metabolism. Some people are prone to PUFAs overload while others are more likely to be deficient. Precision nutrition looks at these genetic differences to help individualize supplements and diet (Chilton et al., 2017; Panda et al., 2022).
Food list
Healthy fats include all the following:
- Extra-virgin olive oil (MUFAs)
- Fish and fish oil (omega-3 PUFAs)
- Tahini, nuts, and seeds (omega-6 PUFAs)
- Grass-fed butter, ghee, or coconut oil (saturated fat)
It may take experimentation to find out which fats work best for you and your overall health.
5) Be cautious of plant sterols
Plant sterols are claimed to be “safe” for people with high cholesterol. Many foods are massively fortified with high levels of plant sterols, such as margarine, and spreads. We are consuming more plant sterols than ever before in history!
Contrary to mainstream advice, new research reveals that plant sterols should not be recommended to most people. The potential harms of mass fortification with these compounds are now coming to light (Makhmudova et al., 2021; Helgadottir et al., 2020).
Scientists caution that plant sterols may build up in blood vessels and increase the risk of heart disease (Makhmudova et al., 2021; Helgadottir et al., 2021; Helgadottir et al., 2020).
Read more about the dangers of plant sterols:
6) Don’t forget these overlooked nutrients
The mineral matrix
The sum of all the minerals that we are taking in through our diet and that build our tissues have recently been termed the mineral matrix.
Nutrients that play vital roles in heart health but are lacking in our diet include magnesium and copper.
Magnesium
Most people know that magnesium is a key nutrient for the heart, with higher levels linked with better heart health. People with higher magnesium intake tend to have a lower risk of metabolic syndrome, diabetes, high blood pressure, and stroke (Rosique-Esteban et al., 2018).
Magnesium deficiency is common—about 10%–30% of the population don’t have enough magnesium in their body for optimal health. Many cases go undiagnosed (DiNicolantonio et al., 2018).
Food list
The best dietary sources of magnesium are (Vormann, 2016; NIH):
- Pumpkin seeds
- Chia seeds
- Almonds
- Cashews
- Spinach
- Whole grains
Copper
Copper is the most overlooked nutrient that many people are deficient in.
Our soil has been depleted of copper due to modern, industrialized agriculture. As a result, foods and livestock are also deficient. We are taking in far less copper than our ancestors did (Hill & Shannon, 2019; Wazir & Ghobrial, 2017).
Copper deficiency is, according to some experts, a major cause of coronary heart disease. It increases the risk of high cholesterol, chronic inflammation, high blood sugar, and oxidative stress. Eating ultra-processed foods and not getting enough copper-rich foods predisposes you to copper deficiency (DiNicolantonio et al., 2018).
Food list
The best dietary sources of copper are (NIH):
- Organ meats (beef liver, turkey giblet)
- Oysters
- Cashews
- Crab meat
- Mushrooms
- Salmon
7) Pay attention to diet quality
Diet quality is a complex concept, but it comes down to a balance of high-quality macronutrients (carbs, proteins, and fats) and micronutrients (vitamins and minerals). It relies on a variety of bioactive-rich, minimally-processed foods—all listed in the previous section (Vanegas et al., 2022).
In a Mediterranean population of over 18k adults, high-quality macronutrient intake was linked with a lower risk of heart disease (Vanegas et al., 2022).
Regarding energy from carbohydrates, both high and low percentages, have been associated with increased mortality. The lowest risk of mortality was between 50–55% of calories from carbs (Vanegas et al., 2022).
8) Avoid processed foods
To ensure diet quality, avoid (Vanegas et al., 2022; Cacau et al., 2022):
- Ultra-processed foods
- Sugars
- Artificial sweeteners
- Refined starch
- Industrial additives
- Trans fatty acids
- Sodium/salt
- Alcohol
- Refined oils
Ultra-processed foods are industrial formulations made entirely or primarily of substances extracted from foods or lab-synthesized ingredients. High ultra-processed food intake is a measure of poor diet quality, and it’s been linked to heart disease (Cacau et al., 2022).
Learn how to read labels and avoid as many processed foods as possible. Many ultra-processed foods are also endocrine/microbiome disruptors. Remember, it’s not just about your heart but about your overall health and wellness.

Read Next:
- 100+ Cholesterol Statistics & Heart Health Facts (2022)
- Benefits of L. Reuteri for Cholesterol
- 4 Root Causes of High Cholesterol (Myths and Facts

Ana Aleksic, MSc (Pharmacy)
Ana is an integrative pharmacist and scientist with many years of medical writing, clinical research, and health advising experience. She loves communicating science and empowering people to achieve their optimal health. Ana has edited 800+ and written 200+ posts, some of which reached over 1 million people. Her specialties are natural remedies, drug-supplement interactions, women’s health, and mental health. She is also a birth doula and a strong advocate of bridging scientific knowledge with holistic medicine.