The basic building block of the human body is the cell. Up to 100 trillion (1014) cells are organized into specialized tissues and organs which comprise the body systems that carry out the functions necessary for survival (e.g., digestive system, cardiovascular system, nervous system, immune system). However, only one tenth of “human” cells are human in origin. The remaining 90% of cells are composed of the microorganisms that colonize our bodies. The lion’s share of these organisms (collectively known as the microbiota) is the bacteria which reside in our gastrointestinal tract. From there, the microbiota exerts a tremendous influence on our body systems, tweaking them in a way that can have a great impact on our health and well-being.
A Community of Microbes
Before we are born, our bodies are essentially sterile. Upon birth, depending on how we were born, we are colonized with the bacteria that reside either in the birth canal or on our mothers’ skin. Shortly after, exposure to the outside environment, handling by parents, diet and genetics help to establish the species that make up the communities of microbes that live in and on our bodies. To say that this community is diverse is an understatement. Scientists estimate that up to 500-1000 different species can colonize the body at one time. Moreover, the human microbiota is an incredibly dynamic and ever-changing collection of organisms. Bacteria are constantly being shed from our bodies via fecal material and introduced via the food we eat and the people and objects we touch. Medications such as antibiotics and certain disease states can also influence microbial populations.Metabolic Potential
Humans and the microbiota have been co-evolving for thousands of years. During this process, the microbiota has developed many ways to break-down and synthesize compounds that can be highly beneficial to our health. To determine how these microbes contribute to our health, scientists study germ-free animals. These animals, usually mice, are born and raised in a completely sterile environment, and thus have no microbiota. When compared to their normal, colonized counter-parts, germ-free mice have structural defects in their muscle and blood vessel architecture, underdeveloped immune systems, are more susceptible to infection and exhibit reduced digestive enzyme activity. In fact, germ-free animals need to consume on average 30% more calories than colonized mice in order to maintain the same body weight. This difference is minimized when the germ-free mice are colonized with members of the microbiota, suggesting that bacteria contribute to the digestion of food stuffs. Another way to study the impact of the microbiota on host physiology is to look at dysbiosis —the shift in microbial populations associated with various disease states. Several metabolic diseases such as obesity, type 2 diabetes, inflammatory bowel disease, cardiovascular disease and even some forms of cancer are associated with changes in the resident microbiota. For example, obese individuals tend to have a lower proportion of a class of bacteria called Bacteriodetes than their leaner counterparts, and a lower incidence of another type of bacteria, Firmicutes, is observed in people with type 2 diabetes than in non-diabetics. The composition of the microbiota can also be shifted in a direction that promotes health (probiosis). This concept was central to the ideas proposed by the Nobel Prize winning scientist Elie Metchnikoff. He noticed that the peasants of rural Bulgaria and Russia consumed a large quantity of fermented milk and enjoyed an exceptionally long life span. He hypothesized that by establishing themselves in the guts of the peasants, the bacteria in the milk were promoting a long, healthy life. Since these observations were made in the early 1900’s, many experiments have supported this view. The bacteria that promote probiosis often originate from the microbiota and are called probiotics. The mechanisms by which the microbiota and probiotics exert their beneficial effects are rooted in the products of bacterial metabolism. Metabolism refers to the series of enzyme-catalyzed chemical reactions that all organisms use to break-down and synthesize organic compounds. When you consider that every member of the microbiota has its own DNA genome, the genetic, and hence, metabolic capacity of humans effectively increases from 25 000 genes to approximately 8 million! Given this huge potential, it is not surprising that the metabolic activities of the microbiota complement our own. Some of these activities include synthesizing vitamins such as vitamins K, B12, folate and biotin; and breaking down sugars, starches, fats, proteins, vitamins, minerals, pharmaceutical drugs and environmental toxins. Basically, the microbiota is only limited by the types of compounds we ingest. The products of these reactions (metabolites) can either be used as energy sources, substrates for other metabolic reactions or as metabolic signals.
Interactions with body systems
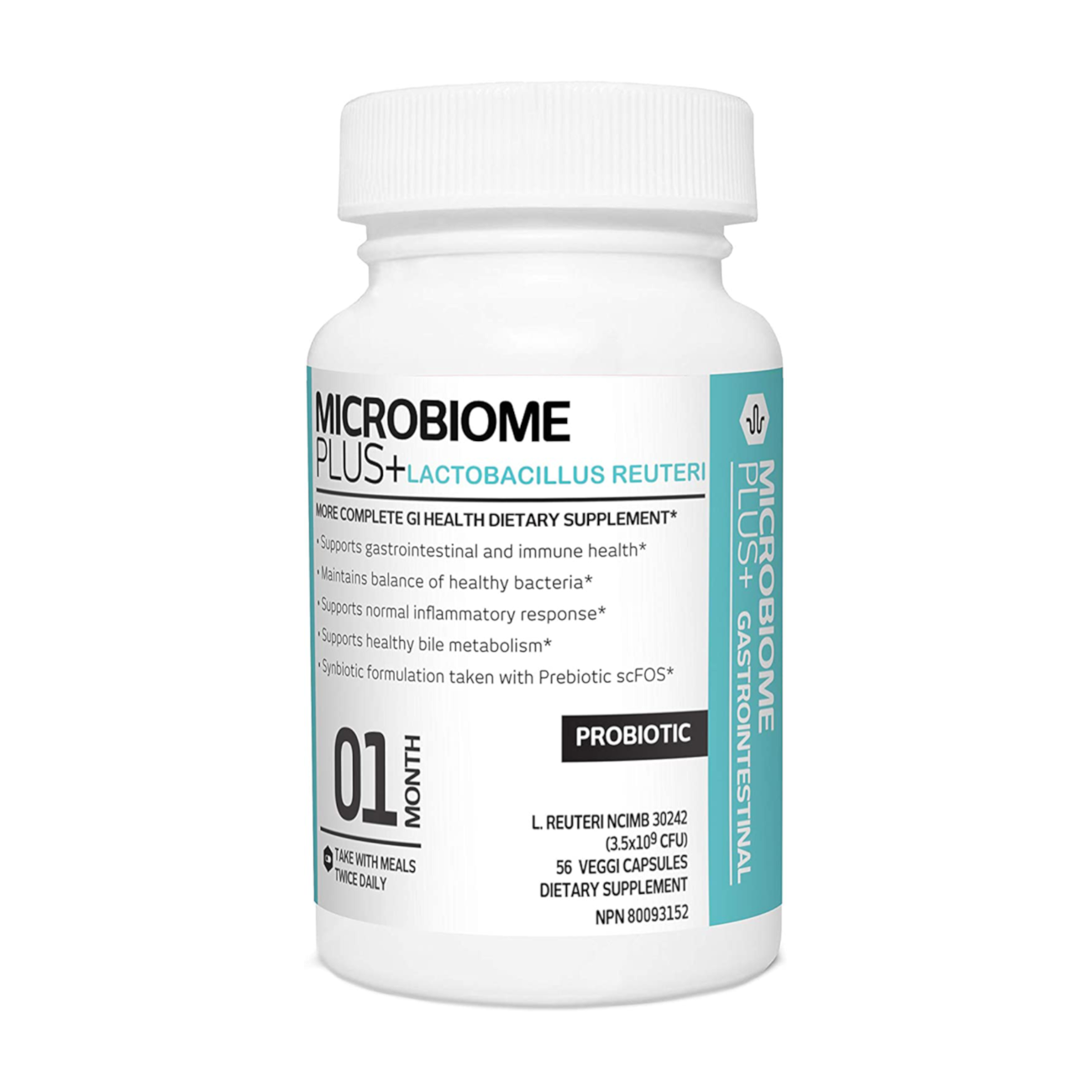
No body system works in isolation, the circulatory system works in concert with the respiratory system to ensure that blood is oxygenated. Similarly the metabolic activities of the microbiota in the gut have far-reaching consequences. Bacterial metabolites, once they are absorbed into the bloodstream, have the potential to act as signaling molecules that can modulate the function of a number of organs and body systems including the immune system, brain, liver and heart. These modulations ensure that target organs are performing optimally. For example, the role of some intestinal bacteria in the break-down of bile acids and the maintenance of heart health has been known for some time. If blood vessels become constricted due to the accumulation of fatty materials such as cholesterol on the vessel wall, a strain is put on the heart as it pumps blood through-out the body and, over time, its function will deteriorate. Bile acids are made from cholesterol. Therefore, the presence of bacteria in the gut with the ability to break-down bile acids reduces the pool of cholesterol available to accumulate in blood vessels ensuring optimal heart function. A recent study showed that when patients with high cholesterol levels were given daily doses of the probiotic bacterium Lactobacillus reuteri NCIMB 30242, their blood cholesterol levels dropped by almost 10% compared to patients that were given a placebo. This study demonstrates the potential of beneficial bacteria to influence our body systems. Indeed, when it comes to the microbiota, we are what they eat. Bacteria in the gut break-down food products into metabolic signals that can affect many body organs and systems.