Overview
Your skin is the largest organ of your body and is continually exposed to environmental, chemical, and microbial challenges. The health of your skin tends to reflect your overall inner-health status and even your age. Glowing skin and shiny hair are unanimous markers of good health. Just like the way experts have been able to reveal a link between our gut and brain, they are also exploring the gut-skin axis and how the health of your gut microbiome will impact the health of your skin. Several skin concerns such as acne, dry skin, rosacea, eczema, psoriasis ̶ you name them ̶ seem to originate from the same root cause ̶ i.e. poorly functioning gut and microbiome.
Here, we’ll learn about how the two systems – gut and skin – function in unison with one another.
People suffering from skin diseases are prone to develop GI distress
A study involving over 13,000 teenagers showed that those with acne were more likely to experience digestive complaints like constipation, abdominal bloating, gastric reflux, and bad breath. The researchers concluded that poor gut function is a major risk factor for skin diseases and such individuals will eventually develop one or more skin diseases. [1]
Another essential pointer towards the link between gut and skin health is the high rate of GI diseases such as SIBO, inflammatory bowel disease, IBS, and H. pylori infection in rosacea sufferers. One study showed that rosacea sufferers were 13 times more likely to suffer from SIBO. Even more remarkable was the finding that treatment of the SIBO with antibiotics healed rosacea in 40 individuals. [2] Diet may also influence rosacea via the gut-skin link. [3]
Leaky gut and altered microbiome may be the culprit behind skin diseases
The acne sufferers tend to display a leaky gut and an imbalanced gut flora, both of which cause skin inflammation and disease. The early nineteenth century scientists reported that the stomachs of nearly 40% of acne sufferers have a minimal to absent hydrochloric acid (HCl) production. This subsequently causes the colonic bacteria to migrate to the small intestine, disrupting the composition of colonic microbial residents. Hence, recent experts have now identified low HCl production as a significant source of small intestinal bowel overgrowth (SIBO), which in turn, compromises the gut barrier. The outcome is widespread inflammation, including inflammation of the skin. [4]
In short, low HCl levels in people with acne stimulate SIBO, which causes leaky gut and worsens skin inflammation.
Gut, Brain, and Skin are Connected
People with acne also have a tendency towards developing mental illness and vice versa, further implicating the role of the gut-brain-skin axis. Emotional problems like depression and anxiety could change the normal composition of the gut microbiome, aggravate the leaky gut syndrome, and thereby, drive the widespread skin inflammation. [5]
Probiotics benefit acne, eczema, and allergic skin diseases
Oxidative stress, a process that generates highly reactive oxygen species, plays an important role in triggering acne. [6] Latest research shows that the beneficial bacteria may slow down the oxidative stress and the subsequent inflammation in skin diseases. Moreover, probiotics can alter the microbial composition at sites other than the gastrointestinal tract such as the skin, implying their significance in tackling skin issues. [4] Last but not the least, the probiotic bacteria may even improve the barrier function of the skin and minimize the skin sensitivity in diseases like rosacea and acne. [7]
Summary
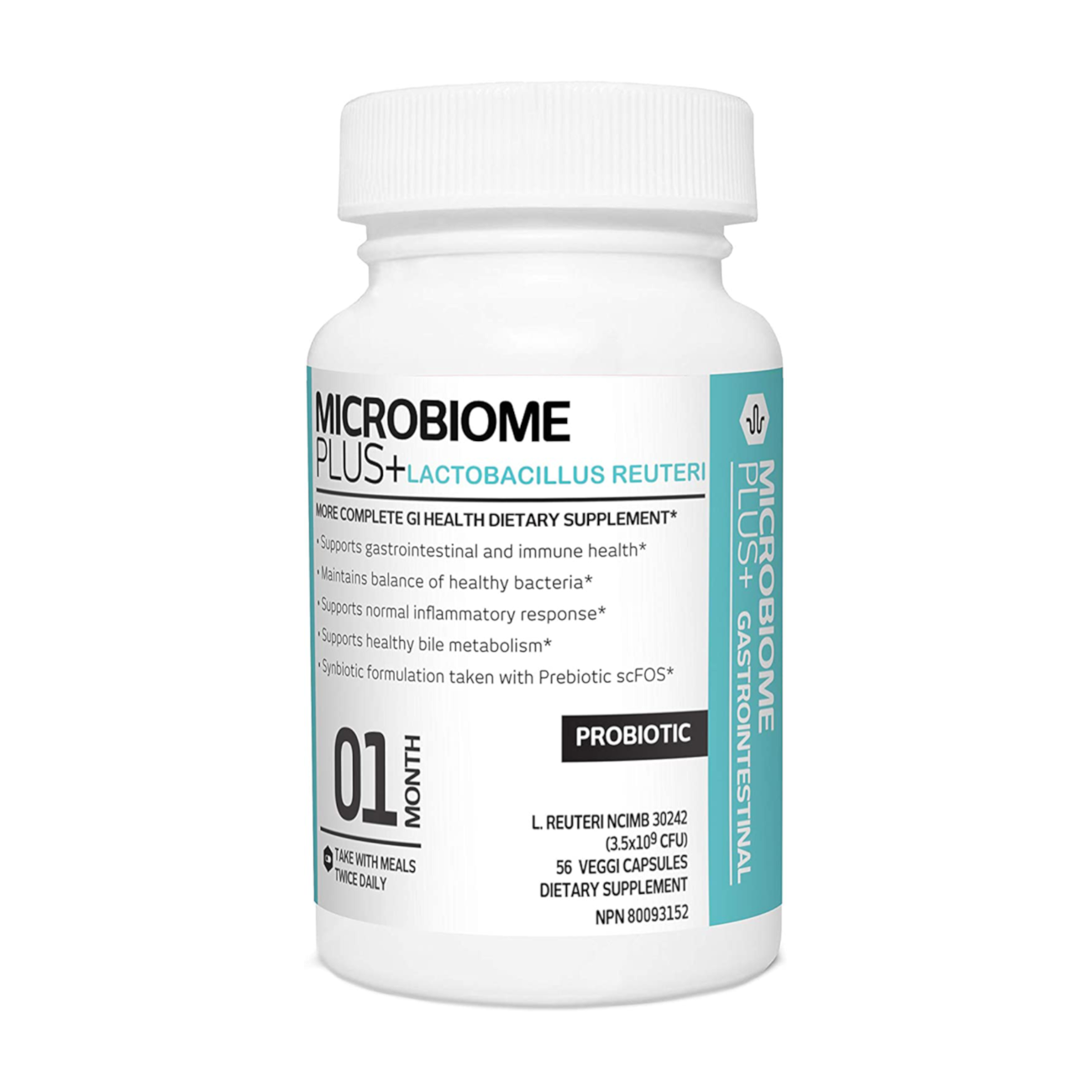
The evidence suggesting the connection between skin and gut health is convincing. Improving the gut health by consuming a healthy diet and supplementing probiotics and fiber-rich prebiotics may be one of the novel treatments for alleviating skin disorders.
References
- Zhang H, Liao W, Chao W et al. Risk factors for sebaceous gland diseases and their relationship to gastrointestinal dysfunction in Han adolescents. J Dermatol. 2008;35(9):555-61. doi: 10.1111/j.1346-8138.2008.00523.x.
- Drago F, De Col E, Agnoletti AF et al. The role of small intestinal bacterial overgrowth in rosacea: A 3-year follow-up. J Am Acad Dermatol. 2016;75(3):e113-e115. doi: 10.1016/j.jaad.2016.01.059.
- Weiss E, Katta R. Diet and rosacea: the role of dietary change in the management of rosacea. Dermatology Practical & Conceptual. 2017;7(4):31-37. doi:10.5826/dpc.0704a08.
- Clark AK, Haas KN, Sivamani RK. Edible Plants and Their Influence on the Gut Microbiome and Acne. Jeong W-S, ed. International Journal of Molecular Sciences. 2017;18(5):1070. doi:10.3390/ijms18051070.
- Bowe W, Patel NB, Logan AC. Acne vulgaris, probiotics and the gut-brain-skin axis: from anecdote to translational medicine. Benef Microbes. 2014;5(2):185-99. doi: 10.3920/BM2012.0060.
- Arican O, Belge Kurutas E, Sasmaz S. Oxidative Stress in Patients With Acne Vulgaris. Mediators of Inflammation. 2005;2005(6):380-384. doi:10.1155/MI.2005.380.
- Gueniche A, Benyacoub J, Philippe D et al. Lactobacillus paracasei CNCM I-2116 (ST11) inhibits substance P-induced skin inflammation and accelerates skin barrier function recovery in vitro. Eur J Dermatol. 2010;20(6):731-7. doi: 10.1684/ejd.2010.1108. Epub 2010 Oct 22.